Prostate cancer
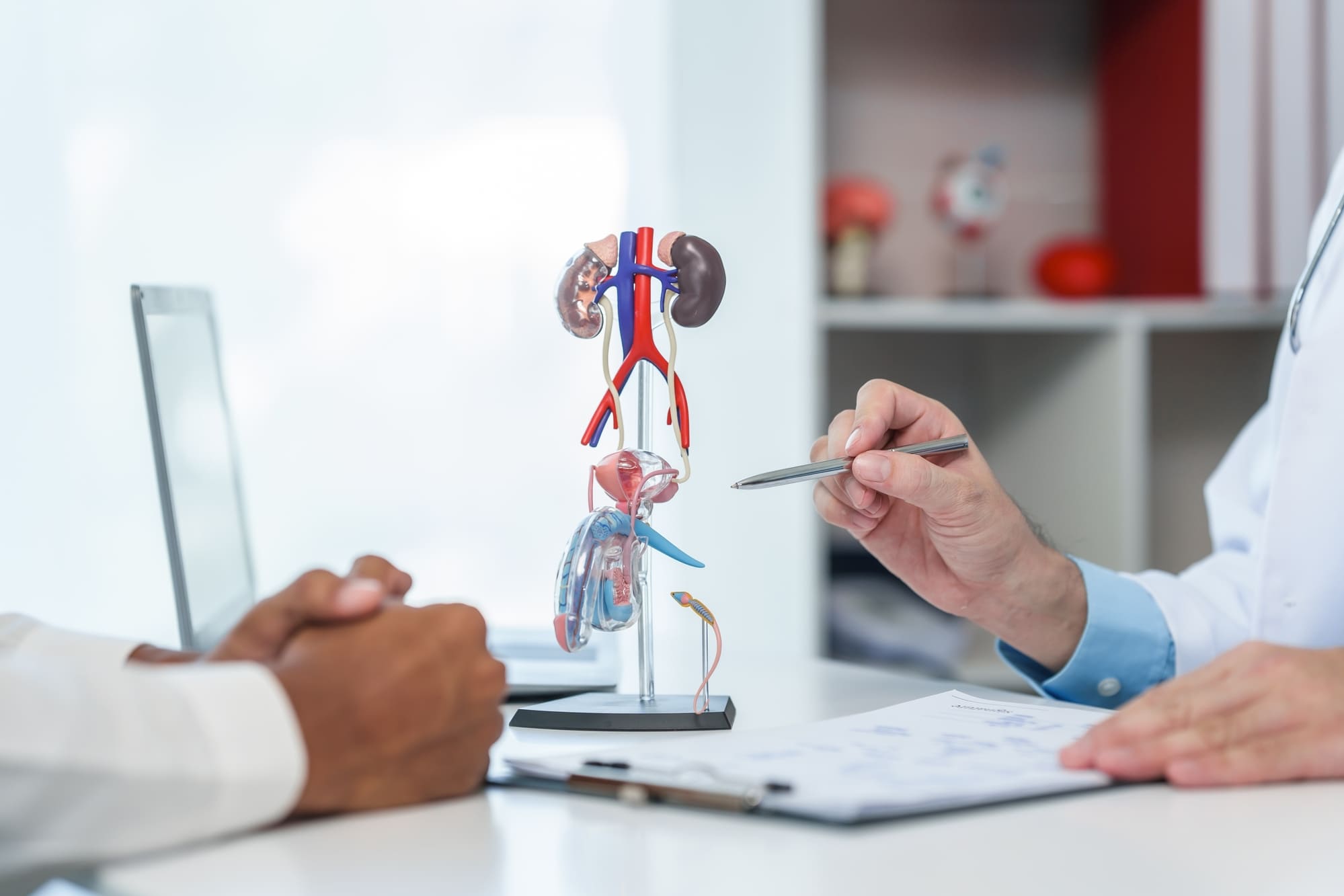
Prostate cancer treatment depends on several factors such as tumour stage, PSA, biopsy results, imaging, prostate volume, urinary problems and individual preferences. These are best discussed in a one-on-one consultation, usually lasting about an hour, to decide the individual treatment.
Patients come to us with medical reports and images for a conversation and discussion. Patients present either with a recommendation from a multidisciplinary tumour board, their urologist or for a second opinion.
Our treatments are guided by innovation and delivered with deeply human care. Experience precision medicine in a place where you are truly seen and supported.
*Mandatory fields
Specialists in prostate care
Led by Prof. Dr. Michael Pinkawa with over 20 years of experience, radiotherapy and brachytherapie at WEGE Klinik is performed by an interdisciplinary team, combining technical precision and compassionate care. Find out about our team.
Treatments at WEGE
Localized prostate cancer is generally classified as low, intermediate, or high risk, depending on individual risk factors. In low-risk cases, active surveillance may be the best option, especially with low number of positive cores. Standard active treatments are radical prostatectomy or radiotherapy. There is no general advantage of one method over the other concerning tumour control (cure). Radiotherapy has advantages of being non-invasive or minimally invasive, and is associated with less impact on quality of life, in particular lower incontinence rates and lower erectile dysfunction rates.
Radiotherapy for prostate cancer includes two established methods: external beam radiotherapy (EBRT) and brachytherapy. According to national and international guidelines, patients should be informed about both options.
External beam radiotherapy (EBRT)
External beam radiotherapy (EBRT) is commonly used as single modality in most radiotherapy departments.
It uses a linear accelerator to deliver radiation from outside the body.

External beam radiotherapy (EBRT) is commonly used as single modality in most radiotherapy departments. It uses a linear accelerator to deliver radiation from outside the body.
External beam radiotherapy as single modality might be the best option for patients with a prior transurethral resection of the prostate, more favourable cancers, larger prostates or increased urinary problems at presentation. External beam radiotherapy is applied as a so called volumetric modulated arc therapy (VMAT), delivering the dose during continuous rotation of linear accelerator gantry around the patient and continuous movement of the leafes that are forming the beam from the respective direction.
Image-guided radiotherapy
It is essential for precise targeting.
An optimal patient preparation before radiotherapy and precise organ localization before each treatment is essential for an effective treatment, exactly delivering the dose to the cancer with best posible protection of the neighbouring healthy tissue.
Spacer application for rectum protection
As the prostate is in immediate neighbourhood to the rectal wall, the rectal wall is always included in the high dose volume in external beam radiotherapy. The consequence is a higher risk of rectal complications, as rectal bleeding or ulcerations, and a significantly decreased bowel quality of life after radiotherapy.
At WEGE Klinik, a hydrogel spacer (SpaceOAR) is injected between the prostate and rectal wall transperineally under transrectal ultrasound imaging, ensuring a 1cm distance between the prostate and rectal wall. The hydrogel spacer remains stable for 3 months and consecutively resolves without any additional interventions.
Prof. Pinkawa was an investigator in the first clinical study with the hydrogel spacer and performed the first injection worldwide in clinical routine in 2010, thus having the longest worldwide experience for this procedure. In the last 15 years, many studies have been published, including a large randomized study, reporting a significant bowel quality of life advantage for radiotherapy after spacer placement in comparison to conventional radiotherapy without a spacer. Bowel quality of life remains the same as bowel quality of life before treatment in patients treated with a hydrogel spacer. More detailed analyses also report improved sexual quality of life in comparison to conventional radiotherapy, thus a higher probability of erections sufficient for sexual intercourse.
For an optimal visualization of the anatomy with the hydrogel spacer, a computed tomography amd magnetic resonance imaging are performed for treatment planning at WEGE. Fusion of both imaging methods in the planning improves the definition of the prostate and the spacer in comparison to conventional treatment planning that is based only on computed tomography.
Brachytherapy
Brachytherapy is based on placement of radioactive sources directly into the prostate, either permanently (LDR brachytherapy, low-dose-rate, applying Iodine-125-sources) or temporarily (HDR brachytherapy, high-dose-rate, applying an Iridium-192-source).

Brachytherapy is based on placement of radioactive sources directly into the prostate, either permanently (LDR brachytherapy, low-dose-rate, applying Iodine-125-sources) or temporarily (HDR brachytherapy, high-dose-rate, applying an Iridium-192-source).
The consectutive advantage is a high biological dose in the tumour without penetration of the skin and other neighbouring organs, thus high dose conformality with a steep dose decline around the prostate.
Brachytherapy can be used as single modality for low risk or favourable intermediate risk patients, usually as LDR brachytherapy. This includes a single procedure of about 1 hour duration and an overnight stay in WEGE. In patients with specific risk factors, reduced dose/duration external beam radiotherapy is combines with brachytherapy as a boost, usually applied in two fractions as HDR brachytherapy.
Clinical studies show that this combined approach improves tumor control, reduces metastasis risk, and may improve survival compared to EBRT or surgery alone.
Prof. Pinkawa, who introduced this method into clinical practice in 2010, has the longest experience worldwide with the spacer. Clinical studies confirm that it significantly reduces bowel side effects and improves quality of life—both gastrointestinal and, in many cases, sexual. Planning with both CT and MRI ensures precise definition of the prostate and spacer, improving the safety and accuracy of treatment.
Image-guided radiotherapy
An optimal patient preparation before radiotherapy and precise organ localization before each treatment is essential for an effective treatment, exactly delivering the dose to the cancer with best posible protection of the neighbouring healthy tissue.
During the brachytherapy procedure, the applicator needles are placed during continuous visualization of the prostate with a transrectal unltrasound. For external beam radiotherapy, external imaging methods need to be used every day to localize the prostate.
Commonly, three gold fiducials are implanted transperineally with a transrectal ultrasound guidance into the prostate before treatment planning imaging for external beam radiotherapy. With the ExacTrac Dynamic system (Brainlab), these fiducials are localized at the treatment table with a dedicated x-ray system that identifies these fiducials and adapts the position of the treatment table in all six directions (including tilting in all directions). Even applying a cone beam computed tomography at the linear accelerator, these fiducials increase the positioning precision significantly.
What is prostate cancer? |
Anatomy and function of the prostate |
How prostate cancer develops |
Symptoms and risk factors |
|---|---|---|---|
|
Prostate cancer is a disease that develops in the prostate gland, a small organ located below the bladder in men. This type of cancer is one of the most common among men and often grows slowly. In its early stages, prostate cancer may not cause noticeable symptoms, making regular check-ups essential for early detection. |
The prostate is a small gland located just below the bladder and in front of the rectum. It surrounds the urethra, the tube that carries urine and semen out of the body. Its main role is to produce seminal fluid, which supports and transports sperm. This function is regulated by male hormones, especially testosterone.
As men age, the prostate often enlarges, which can lead to urinary symptoms. One key marker of prostate health is PSA (Prostate-Specific Antigen), a protein made by the prostate. Elevated PSA levels may signal prostate cancer or other conditions, making PSA testing useful for early detection. |
Prostate cancer usually begins when abnormal cells grow in the gland. In many cases, the cancer grows slowly and may not cause problems for years. However, some forms are more aggressive and spread quickly, requiring prompt treatment.
The growth pattern varies from person to person, so diagnosis and treatment depend on how the cancer behaves in each case. |
Early prostate cancer often causes no symptoms. As it advances, signs may include:
Risk factors include age (especially over 50), family history of prostate cancer, a diet high in fats, obesity, and low physical activity. Regular check-ups help detect the disease early, even without symptoms. |
It depends on the individual case. Around 60–70% of prostate cancer patients receive radiotherapy at some point—either as a primary treatment, after surgery, or to manage symptoms in advanced stages.
This depends on the type of radiotherapy. Standard treatment may require several weeks, while stereotactic radiotherapy can be completed in fewer sessions.
No, the treatment itself is painless. Some patients experience side effects later, but the sessions feel like a regular medical procedure.
Most patients can continue daily activities during treatment. We’ll guide you on managing energy levels and recognizing when to rest.
Side effects may include fatigue, urinary or bowel changes, and temporary sexual dysfunction. These vary by patient and usually improve after treatment.
We use advanced systems like IMRT, VMAT, and stereotactic techniques with sub-millimetric accuracy. This helps spare healthy tissue and reduce side effects.
Testimonials
At WEGE Klinik, we are committed to supporting our patients and their families throughout the prostate cancer journey, offering expert care and understanding every step of the way.
 Markus, 70
Markus, 70
To be honest, I was… kind of scared about the side effects. But the doctors at WEGE Klinik used this hydrogel spacer to protect the area. In the end, the treatment was easier than I expected, and now… I feel like myself again
 Dieter, 68
Dieter, 68
The doctors at WEGE Klinik explained all my options clearly. I chose active surveillance, and I appreciate their careful monitoring and support.
 Jürgen, 62
Jürgen, 62
At WEGE Klinik, we are committed to supporting our patients and their families throughout the prostate cancer journey, offering expert care and understanding every step of the way.
If you have general questions, you can contact us by phone or e-mail. We will then get in touch with you as soon as possible.
WEGE Klinik:
Phone: +49 228 5306 0
Email: info@wegeklinik.com
Web: www.wegeklinik.com
WEGE MVZ:
Phone: +49 228 5306 202
Email: info@wegemvz.com
Web: www.wegemvz.com